As my Twitter followers know from my rant earlier this week, I’ve had medication troubles. Judging from the comments and emails I receive from my readers, you have medication troubles, too. I hope my long, frustrating experience will help you navigate the world of health insurance and stimulant medication. Today, we’ll talk about how you can be denied medication, even if your doctor has already written you a prescription.
I’m putting my whole publication calendar on hold to make room for a tutorial & sternly worded letter template re: dealing w/ Rx authorization if you have #ADHD / #AdultADHD. Because it sucks. Look for it on the blog this week. Meanwhile, rant thread: https://t.co/zJ3tUydeWJ
— Jaclyn Paul (@jaclynleewrites) February 26, 2018
Before we begin, a reminder about me: I’m pretty crunchy, but I love science. You won’t see me take over-the-counter cold medicine, I refuse antibiotics unless they’re absolutely necessary, I ferment my own yogurt…you get the idea. When it comes to ADHD, I’m pro-medication*. Scientific research supports it, and my personal experience supports it. I’ll talk more about that in a future blog post. For now, know that’s my position, and it’s not up for debate in this post.
What is up for debate is how we manage access to these medications. This has much to do with how we view them as a society, and it has to change.
*I feel comfortable advocating for treatment of ADHD with medication because I speak from my own research and experience, not from any material benefit I receive for saying so. I have a strict policy of never accepting any perks, monetary or otherwise, from pharmaceutical or supplement manufacturers.
Even with a valid prescription, you may have trouble getting your ADHD medication
Even if your doctor prescribes a specific medication — one you’ve arrived at through months, or even years, of trial and error — your health insurance reserves the right to say no, or at least to ask for what they call prior authorization.
Prior authorization (PA) is a cost-saving measure for your insurance carrier. When they require PA, they ask your doctor to get approval from them before you fill your prescription. PA gives them one last chance to make sure you won’t (or can’t) use a cheaper alternative.
Generally, you learn you need PA when you try to fill your prescription at the pharmacy. The insurance carrier kicks it back to your pharmacist, who then contacts your doctor to begin the process. When this happened under my previous carrier, I didn’t get involved, and I received my medication that same day. This time, the pharmacist couldn’t reach my doctor’s office because they’d closed for the day.
And so began my week-and-half-long saga.
That’s right: it took me almost two weeks to fill my prescription. The delay was especially long due to a chain of bureaucratic inefficiencies and screw-ups, but I have a bigger beef: I shouldn’t have received the PA request in the first place.
What’s the solution?
My advice to you: be proactive. Stay on the lookout for potential issues, especially around the beginning of the year, and especially if you just changed insurance carriers. Keep your own list of which medications you’ve tried. Include dates, names of drug manufacturers (you can find this on your prescription bottle), and notes on their effectiveness. If your doctor receives a questionnaire like mine did, follow up with your insurance immediately to make sure they received it. Never assume everything is being taken care of. Do your best to head off any issues before you’re out of meds.
Of course, this is only the best we can do with what we have: a system that seems bent on derailing us at every turn.
Below is my letter to my insurance carrier about why this system doesn’t make sense for people with ADHD. Feel free to copy and modify it for your own use.
My letter to my insurance carrier
Hi there. I’m writing to you about my recent experience refilling a prescription that required prior authorization (PA). The medication (Concerta) treats adult attention deficit hyperactivity disorder (ADHD).
As both a [*****] customer and a blogger who writes for adults with ADHD, I have significant concerns about how [*****] handled this situation. Imagining my readers in my shoes, I suspect many would’ve given up before getting the medication they needed.
That this was not addressed urgently, and that I received this request for PA at all, reflects a lack of sufficient information about ADHD and why these medications matter. It also exposes an inefficient system for managing health care costs and claims.
I won’t waste space with the details of my specific experience, except to say a string of bureaucratic mishaps caused a lengthy delay in my prescription refill. I spent nearly two weeks resolving the issue, during which time I ran out of my medication.
In this letter, I want to address concerns about the process as a whole, including a mailer I received about [*****]’s Step Therapy Program. It included the following chart, categorizing ADHD medications from Step 1 (most preferable) to Step 3 (least preferable):
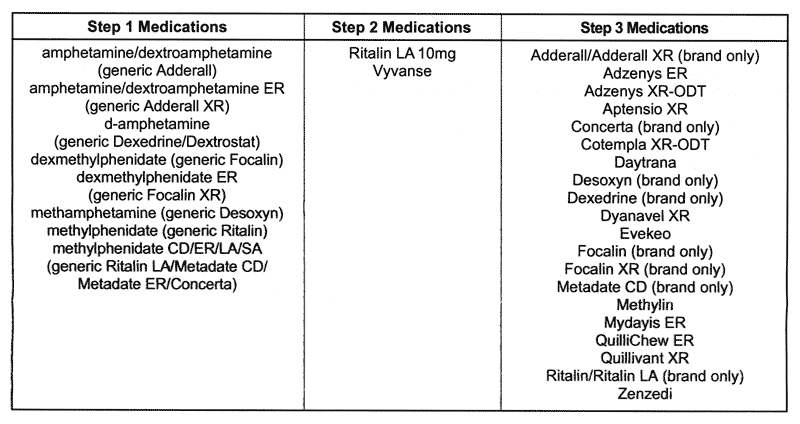
This chart clearly reflects what [*****] would prefer to pay for, but disregards actual patient needs and outcomes. Medication choice for ADHD is highly individualized. There is no one best medication type and dosage for everyone. Doctors and patients can work together for months, if not years, to arrive at an ideal solution. This chart has no bearing on which drugs might be advisable for a patient to try first (or last).
Even so, my medical record clearly shows I have tried several medications from Step 1 and Step 2. A more streamlined system might’ve used this data to bypass a cumbersome PA process based on faxes and telephone calls. (My doctor’s office — and I’m sure many others — doesn’t deal with online forms for these issues.)
It may also have prevented me from running out of my medication. The stimulant refill process requires me to request a new prescription only days before I run out. This leaves no room for delays. I was left to wonder: would I have been treated this way if I had a prescription for blood thinners? Antidepressants? Thyroid medication? Insulin? I suspect not.
And there’s the rub: it seems running out of a stimulant medication isn’t considered an urgent concern. But for adults trying to be safe drivers, productive workers, and responsible parents, the impact can be severe. In the long term, barriers to effective medication for ADHD likely prove more costly to insurers than covering a name-brand medication.
Also important to note: [*****]’s Step Therapy Program letter states that “generics have the same quality, strength, purity, and stability as their brand-name counterparts.” This is untrue, and incredibly misleading to your customers. Per the FDA, a generic drug is “bioequivalent” if its effect falls within 80-120% of the brand’s. When you’re talking about something as complex and sensitive as the human brain, this 40% window is significant. Even worse, the FDA was forced to downgrade generics of the popular drug Concerta (the one I was trying to refill when I encountered my PA issue) when a flood of complaints revealed that they failed to meet bioequivalency standards.
Generic manufacturers have struggled especially hard to replicate Concerta’s unique release mechanism. However, my experience and that of many others will tell you that even generic versions of Ritalin — the oldest, most tried-and-true ADHD drug — are simply not the same. The quality and effectiveness can vary greatly between manufacturers.
Because there are currently no bioequivalent generic alternatives, Concerta shouldn’t be included in Step 3 at all. It should be in Step 1 until there is a viable alternative. [*****] customers shouldn’t be subjected to PA requirements or price penalties to use the name-brand drug.
Health insurance carriers should make it easier, not more difficult, for people with legitimate ADHD diagnoses to access these medications. Improperly treated ADHD contributes to many costly conditions for insurance carriers: obesity, auto accidents, lack of preventative care and wellness checkups, smoking, sexually transmitted diseases, lack of exercise, and excessively risky behavior. Some research shows reduced substance abuse disorders in people whose ADHD is properly treated with stimulant medication. People with ADHD are also at a five-fold risk for self-harm. Insurance companies like [*****] would be wise to help customers avoid these damaging situations.
For many reasons, treatment of ADHD is a complex process. However, effective treatment reduces costly health conditions over the lifespan. For the majority of people with ADHD, effective treatment begins with the correct stimulant type and dosage — a solution they arrive at through a careful process with their health care provider.
Please consider refining your process for approving stimulant drug prescriptions. For so many people with ADHD, these prescriptions are the result of many months or years of struggle. This is documented in our medical records. We don’t need another barrier. We need support to create the conditions for long-term good health.
Sincerely,
Jaclyn Paul
The ADHD Homestead
Hey there! Are you enjoying The ADHD Homestead?
Here's the thing: I don't like ads. I don't want to sell your attention to an advertising service run by the world's biggest data mining company. I also value my integrity and my readers' trust above all, which means I accept very few sponsorships/partnerships.
So I'm asking for your support directly. For the cost of one cup of coffee, you can help keep this site unbiased and ad-free.
Below you will find two buttons. The first lets you join our crew of Patreon pals and pledge monthly support for my work. Patrons also have access to my Audioblogs podcast. The second takes you to a simple donation page to pledge one-time or recurring support for The ADHD Homestead, no frills, no strings. Do whichever feels best for you!